If you notice your leg skin is changing color and taking a reddish-brown tinge, do not take it lightly, as it may be a sign of vein disorder. Discoloration of the lower legs is mainly caused by hemosiderin, which indicates leakage of red blood cells through the veins due to blood vessel conditions and ineffective blood circulation. At Downtown Vein & Vascular Center, Dr. Sergei A. Sobolevsky focuses on diagnosing if your skin discoloration is resulting from some venous disorder or it is a side effect of varicose veins treatment. The top-rated endovascular specialist examines your legs carefully, analyzes your symptoms, and determines their causes to suggest the most appropriate treatment to help you feel and look better as soon as possible.
What Is Hemosiderin Staining?
Hemosiderin staining is the darkening or discoloration of the skin. It appears as a patch of skin, which is a few shades darker than the surrounding skin. It can look like bruising, or it can be reddish-brown or rust-colored. It is also known as hemosiderin deposition or hemosiderin hyperpigmentation.
Hemosiderin staining becomes harder to spot if you have a dark skin tone. If left untreated, this discoloration may become darker and look nearly black. Hemosiderin staining usually happens on the lower leg, near the ankles, or the feet. It is caused by blood leaking out of the tiny vessels called capillaries. The blood pools under the skin and leaves a residue of hemoglobin that settles in the tissue there. Hemoglobin contains iron, which causes the rusty color of the stains.
Read more: Should I Be Concerned About Dark Veins?
What Causes Hemosiderin Staining?
Hemosiderin staining occurs when red blood cells leak through the veins, and iron or other byproducts are released. It can happen for several reasons. As a result, a brown stain shows up on the skin, creating a reddish-brown or bruise-like appearance.
The white blood cells or immune system can clear up some of the excessive iron released into the skin, but certain medical conditions overwhelm this process, resulting in skin discoloration or staining.
Some common conditions associated with hemosiderin staining include:
- Trauma
- Leg edema
- Diabetes
- Cardiovascular disease
- High blood pressure
- Venous ulcers
- Venous hypertension
- Vein insufficiency
- Lipodermatosclerosis, a skin, and connective tissue disease
- Vein treatments
In addition to its unsightly appearance, hemosiderin staining indicates an underlying health condition. The reddish-brown discoloration on the lower legs is caused by the abnormal functioning of veins.
If hemosiderin staining has occurred as a side effect of skin injury or treatments, chances are it will clear up on its own. Staining due to heart disease, vein disease, or chronic wounds often remains. The pigment may lighten over time, but not in all cases.
Read more: 4 Things You Must Know Before Accepting a Lipedema Treatment
Hemosiderin Staining and Varicose Veins
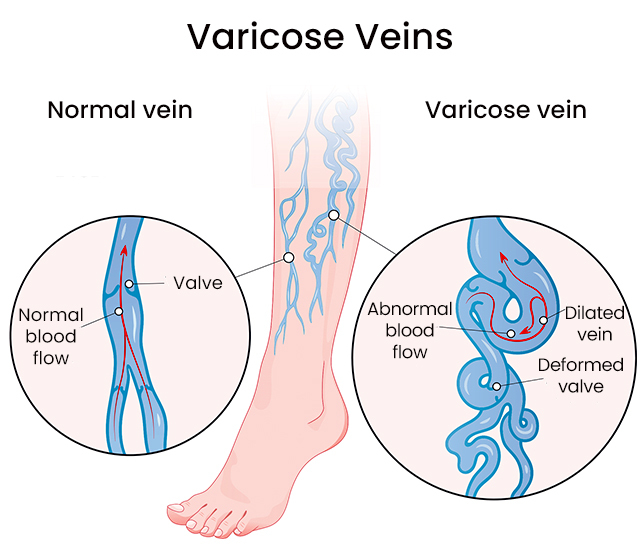
Changes in the color and texture of the skin are one of the complications of varicose veins in which your veins become enlarged and twisted. Skin discoloration from varicose veins occurs at an advanced stage of venous insufficiency, when the veins fail to function correctly, causing blood to pool in the lower areas of the legs. When the blood stays there, it leeches iron into the skin and causes skin discoloration.
The longer you delay treatment for your varicose veins, the more staining or discoloration you will experience, and the more likely it is for the discoloration to become permanent.
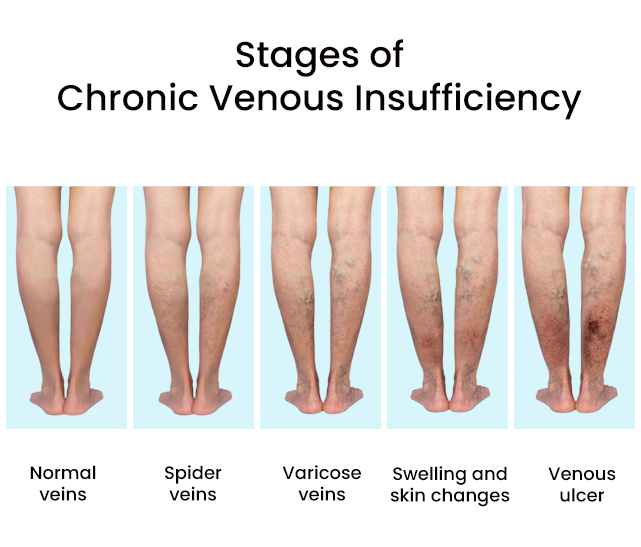
Chronic Venous Insufficiency and Hemosiderin Staining
Hemosiderin staining is usually a symptom of a condition in the blood vessels in your legs called chronic venous insufficiency. Veins are the vessels that carry blood back to the heart from the rest of your body. The veins in the legs have one-way valves that keep the blood from flowing backward, away from the heart. Chronic venous insufficiency occurs when these valves fail to function normally. Instead of flowing upward as it should, blood begins to pool in the legs and feet.
The iron in the blood leaks through the vein walls and stains the skin, leading to hemosiderin staining. This skin discoloration does not go away unless its source or the diseased vein is addressed.
Chronic venous insufficiency is not serious on its own, but it can lead to other uncomfortable symptoms and make it harder to accomplish daily goals. Symptoms include:
- Pain and fatigue in the legs
- Swelling, especially after long periods of sitting or standing still
- Cramps
- Varicose veins
- Itching or flaking skin
- Sores that do not heal
Your risk of developing chronic venous insufficiency increase if:
- You are a female in case of hormonal imbalances
- You are pregnant
- You have been through multiple pregnancies
- You have had an injury that affected the veins in your legs, such as surgery, a car accident, or a sports injury
- You have a family history of varicose veins
- You are growing old and have certain other medical conditions
- You lead a sedentary life without any physical activity or exercise
If you notice discoloration on your legs or hemosiderin staining, seek medical attention right away. CVI can be treated if detected at an early stage with a combination of non-invasive and surgical procedures. Timely diagnosis and treatment can halt the vein disease progress and prevent discoloration. In some cases, the staining will disappear completely.
Read more: How to Tell If You Need a Lymphatic Drainage Massage
Skin Discoloration Caused by Varicose Vein Treatment
Many people experience hemosiderin staining or leg discoloration after seeking treatment for varicose veins. Sclerotherapy involves injecting a chemical solution, known as a sclerosant, directly into the varicose or spider vein. The solution causes the vein walls to swell, stick together, and seal shut, stopping the flow of blood.
Sclerotherapy procedures reduce symptoms associated with varicose veins, as well as improve the physical appearance of the affected areas, but it may lead to hemosiderin staining at the site of injection. The staining is of a blueish-brown hue and often observed along the pathway of the treated veins. Patients often describe staining or darkening as a shadow of where the treated veins were once. This discoloration is usually temporary and disappears in a couple of weeks, but for some people, the stain ends up being permanent.
There are certain other factors too that increase the possibility of hemosiderin staining. They include:
- Skin with increased melanin
- Unprotected sun exposure
- Sensitive skin
- Certain medications
- Keloid scarring from prior procedures or injury
- People who have thin skin
There is no definite way to predict who will have staining. Even if you notice skin discoloration after sclerotherapy, there is no need to worry as it indicates the treatment is working and the damaged veins are shutting down. Also, this type of staining is not permanent, and will fade with time.
Is It Possible to Treat Hemosiderin Staining?
It is essential to consult a doctor to find out what is causing your symptoms and the best treatment options. If hemosiderin staining is the result of vein disease, it is necessary to treat the cause and not just the symptoms. The goal of the treatment is to address the condition causing the discoloration.
Hemosiderin staining can be treated effectively with topical lotions and ointments. In case they don’t work, the doctor may suggest minimally invasive procedures and surgical options that lighten the skin. Laser treatment or intense pulsed light (IPL) help to lighten the dark spots on the skin.
Despite how your legs may appear following treatment, most patients report significant improvement in their symptoms. As your symptoms of vein disease lessen, your legs will look better shortly after.
What to Expect After Treatment for Varicose Veins
Varicose veins take years to form. They just do not pop, enlarge or swell overnight. In the same way, they will not go away overnight. Give your body time to heal and break down treated veins. Even if you bump your leg against something hard and get a nasty bruise, it takes a few weeks to heal. The larger the bruise, the longer time it takes to heal. The same is the recovery process of diseased veins. The larger or more damaged the vein, the longer it will take your body to break down and heal, while smaller veins will take less time.
If your skin discoloration is an outcome of sclerotherapy vein treatment, you will need touch-up treatment. The vein specialist keeps an eye on your recovery process and calls you for a follow-up after the procedures to ensure all diseased veins have been treated.
As the large branches of veins are treated, the blood is diverted into smaller subdivisions that can attempt to feed into closed segments of the vein. This creates pressure or discomfort and is referred to as trapped blood, as this blood sits in that spot of the vein and causes hemosiderin staining. The specialist fixes this problem by injecting the diseased veins and draining trapped blood to help you look and feel better as soon as possible. Also, as your skin cells cast off naturally with time, new skin cells replace them, free of all staining.
Hemosiderin staining is not something that you have to deal with for life. Whether it is resulting from chronic venous insufficiency or varicose veins or its treatment, it is best to seek medical attention if you notice changes in your skin color. Visit Downtown Vein & Vascular Center to discuss your symptoms and the underlying causes behind them with experts. Dr. Sergei A. Sobolevsky is an endovascular specialist with extensive expertise in Image-Guided Minimally Invasive Medicine and Vascular and Interventional Radiology. He uses advanced diagnostic methods to investigate your vein conditions and combines the most effective treatment methods to help you find relief.


