Dark spots on your legs and feet can be a result of a variety of conditions. But if they are not going away on their own or seem to be changing their color or size and turning painful, it may be something that needs medical attention. Proper diagnosis of the underlying cause can help you seek the best treatment to reduce dark spots on the bottom or top of your feet. At Downtown Vein & Vascular Center, Dr. Sergei A. Sobolevsky evaluates the dark spots on your feet, analyzes your symptoms, and figures out what is causing them. He specializes in the diagnosis and treatment of deep venous and arterial diseases of the lower extremities and recommends the best options to alleviate the discomfort resulting from these dark spots.
Marks and bumps are not uncommon. They can appear on any part of the body but are usually found on the legs and feet. Most of these marks and bumps are harmless, but if they don’t seem to go away on their own or worsen, leading to other painful symptoms, call your healthcare provider.
What Causes Dark Spots on the Bottom of the Feet?
Dark spots on the legs and feet are not unusual. Generally, they are bruises or scars that happen to those who work on their feet often or do manual labor. However, a discolored spot without any other signs of bumps or bruising can be a warning sign of something more serious.
According to health experts, two conditions can cause dark spots on the bottom or top of your feet:
- Venous stasis dermatitis
- Malignant melanomas
Both these conditions can cause discolored spots along with additional symptoms like pain and swelling to the foot and ankle. If you are observing any unusual new and dark spots on the bottom or top of your feet, call your doctor for proper diagnosis and timely treatment.
What Is Venous Stasis Dermatitis?
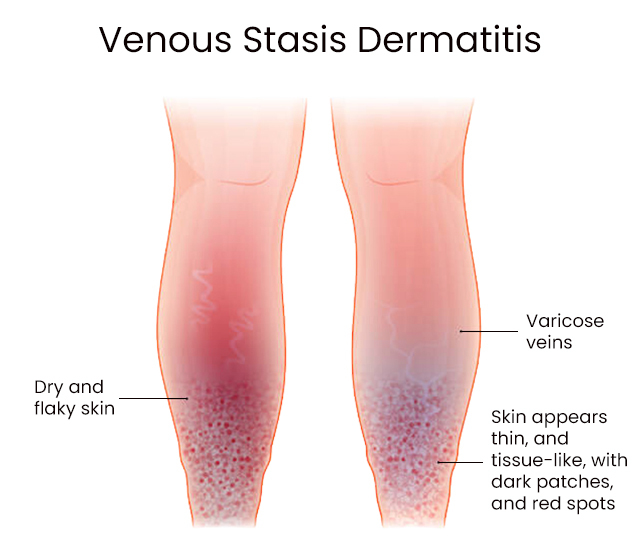
Venous stasis dermatitis occurs when blood begins to pool in the lower legs and puts pressure on the skin. Too much strain leads to pain, discoloration of the skin, itching, and sores. This condition happens due to some venous disease when the blood does not move through the veins properly, either due to a blockage or other pressure inside the veins. Sometimes, it is also a warning sign of medical conditions like kidney or heart disease.
Stasis dermatitis is also known as gravitational dermatitis and venous eczema. It is most common in people above the age of 50, but it can occur in younger people too. Also, it is more frequent among women than men. Fortunately, venous stasis dermatitis can be treated and managed with medication, special bandages, and self-care.
Symptoms
Swelling around the ankles is one of the first symptoms you will observe. It may get better as you sleep when the legs are elevated, but it comes back when you are active during the day. Your legs will feel heavy when you walk or stand.
Other common symptoms of venous stasis dermatitis include:
- A yellow, red, or brown coloration to the skin around the ankles and on top of the foot
- Bulging or twisted varicose veins that look blue or purple
- Itching or pain from the discolored area
- Thickening of skin around the affected area
- Sores that release ooze or look crusty or scaly
- Loss of hair from the ankles and shins
Most of these symptoms occur as the condition progresses from moderate to severe. Most people only suffer from swelling and discolored spots on the skin.
Read more: Blue Veins: An Illinois Vein Specialist Explains Why Your Veins Are Blue
What Causes Venous Stasis Dermatitis?
Venous stasis dermatitis occurs as a result of circulation problems when blood begins to collect in the lower leg. This pooling of blood, known as stasis, may be due to chronic vein insufficiency. Veins have valves that keep the blood moving in the right direction. If these vein valves get damaged or stop functioning properly, they can stretch out and hold the blood instead of sending it back to the heart. Blood also begins to collect in veins due to blood clots, an injury, or surgery.
Pooled blood and fluids leak from the veins and put pressure on the skin from the inside. This pressure causes stasis dermatitis symptoms. Stasis dermatitis is common in people with circulation or other cardiovascular issues. As this condition is a venous disease, the causes of symptoms come down to the body’s inability to remove blood from the veins or circulate it properly to other parts of the body.
Several other conditions and factors that increase your chances of getting venous stasis dermatitis include:
- High blood pressure
- Varicose veins
- History of heart failure or kidney failure
- A localized blood clot in the leg
- Being overweight or obese
- History of surgeries in the affected area
- Sedentary lifestyle
- Sitting or standing in one place for long hours
- Multiple pregnancies
Treatment for Stasis Dermatitis
There are several ways to treat venous stasis dermatitis. You may be asked to apply a special bandage or dressing to the affected areas, rub a medicated cream onto the skin, and take antibiotics if you have an infection. Steroids or antihistamines are prescribed to alleviate pain, redness, or itchiness resulting from this condition.
Your doctor may recommend surgical procedures to treat vein disorders if the above treatments do not work. These minimally invasive procedures reroute the blood flow in the leg to reduce the amount of blood trying to move through the insufficient area, preventing the blood from leaking into the surrounding tissue.
You can also keep the pain and swelling down by trying the following at-home care tips:
- Wearing compression stockings
- Keeping your feet elevated above the heart to encourage the smooth flow of blood to the heart
- Getting up and walking frequently to keep the blood moving in the veins
- Relieving dryness or itchiness from scaly spots on the legs by using a good quality moisturizer on the skin.
Do not use a moisturizer or any other medication on open sores, as it can lead to infection or further damage to the tissue. Consult your healthcare provider if your symptoms of stasis dermatitis persist. If left untreated, this condition can also cause permanent changes to your skin.
Discover other treatments our top vein doctors near you in Brooklyn offer:
Malignant Melanoma of the Foot
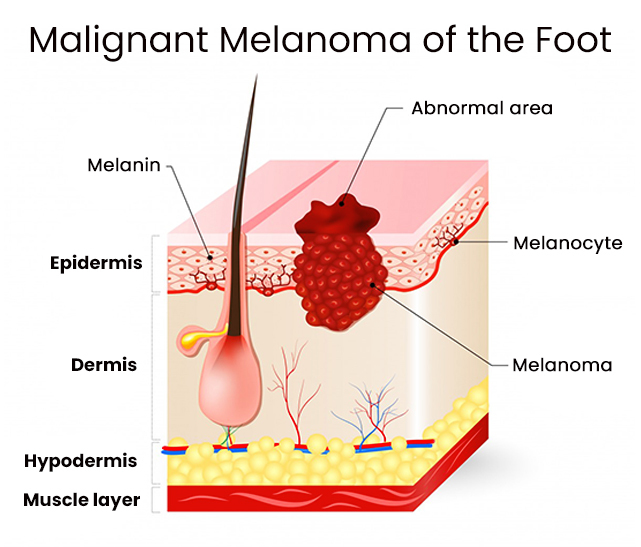
Foot melanoma is a type of skin cancer that starts in the feet. It can appear anywhere on the feet, including the sole or under the nail, and affects the pigment-producing skin cells. It can spread to other parts of the body by referring to the nearby tissue and in the case of the advanced stage, through the bloodstream. If it grows, it can be life-threatening.
Many people may not even notice they have food melanoma because the foot is usually not checked so thoroughly for signs of skin damage. Melanoma is not the only type of skin cancer, but it causes the highest number of deaths of any skin cancer. Luckily, melanoma can be treated if it is detected in the early stages.
Unlike stasis dermatitis, malignant melanomas can appear on any part of the body, including the top and bottom of the foot.
What Causes Melanoma of the Foot?
Most cases of melanoma start due to overexposure to ultraviolet radiation (UV). This radiation is one of the many electromagnetic waves given off by the sun. It is the same radiation used in tanning beds and salons to encourage pigmentation development in the skin. Excessive UV exposure can also turn a noncancerous mole into melanoma. Cells that produce pigment divide rapidly to spread pigmentation, which increases the risk of melanomas.
Anyone can develop melanoma over time, but certain factors can increase the risk of developing melanoma, including:
- Fair and freckled skin
- Lighter hair tones
- Sensitivity to sun
- Occurrence of blistering sunburns before the age of 18
- Presence of numerous moles on the body, especially if they developed before the age of 18
- Preexisting moles on your feet
- Having a family history of melanoma or any other type of skin cancer
Once developed, melanomas appear on the body as dark, asymmetrical spots on the skin. These spots may be brown, blue, or black. They are sometimes red or white too. A number of these colors may also be present in the same spot. None of these discolorations indicate melanoma, but they are visible symptoms of this condition.
Symptoms of Foot Melanoma
The first sign of melanoma is a change in the size, color, shape, or texture of an existing mole or a new mole. Melanoma can increase in size over time from benign moles. If a dark spot on your skin is growing bigger or has an irregular border with adjacent skin, it could be a sign of malignant melanoma. Foot melanoma usually appears on the sole or under a toenail but can appear anywhere on the foot or ankle.
Other warning signs for foot melanoma include:
- A sore that does not heal
- Pigment spreading from the border of a lesion to the surrounding skin
- Redness or a new swelling beyond the border of a lesion
- Changes in sensation, such as itchiness, tenderness, or pain
- Changes in the surface of a mole, including scaling, oozing, bleeding, or the appearance of a bump or nodule
Diagnosing and Treating Foot Melanoma
Cancer of the foot and ankle is not so easy to identify. The doctor will examine your foot for skin changes and ask you about any family history of skin cancer. They will also take a sample of the area for a biopsy. Identifying the cells pulled from the affected region help in making an accurate diagnosis of your condition.
They will also assess the approximate date of the lesion’s development, any changes in the shape and size, additional signs or symptoms such as pain, itching, or bleeding, and the presence of any other suspicious moles. If the doctor suspects melanoma, he will refer you to a specialist for treating skin conditions and cancers.
Read more: Why Are The Veins in My Feet Bulging?
Treatment of Foot Melanoma
Treatment options for foot melanoma depend on the stage of diagnosis as well as your overall health. If diagnosed timely, the doctor may simply cut out the mole and the skin surrounding it. It is called excision and does not take much time.
Advanced cases of foot melanoma may require:
- Chemotherapy — it uses chemicals to kill the cancer cells in your body
- Immunotherapy — it stimulates the immune system to attack cancer cells
- Lymphadenectomy — a type of surgery that removes affected lymph nodes
- Radiation therapy — it uses radiation to shrink tumors
How to Prevent Foot Melanoma
There are several steps you can take to protect yourself from cancer or detect them early.
They include:
- Wear water shoes or socks when going to the beach.
- Use proper protection from the sun, including sunblock, shade, and sun-resistant clothing.
- Remove nail polish and inspect the nails for dark spots.
- Check all areas of the foot and ankle, including between the toes and underneath the foot for any abnormal bump or nodule.
When caught early, food melanoma is easier to treat. It is necessary to look for unusual spots throughout your entire body, including your feet, to prevent life-threatening consequences.
Venous stasis dermatitis and malignant foot melanoma are the two main reasons for dark spots on the bottom or top of the feet. While stasis dermatitis results from age, lack of activity, and faulty valves in the legs, melanomas come from multiple sources, including excessive exposure to the sun, and can happen to anyone of any age. Early detection can help prevent severe symptoms from both afflictions.
Common reasons for dark spots include sun exposure, diabetes, skin cancer, or post-inflammatory hyperpigmentation, but it could be a sign of another health condition. If you are noticing any discolored spots on your foot, call your doctor right away to have them reviewed. Dr. Sergei A. Sobolevsky is a top endovascular specialist and uses the most advanced diagnostic tools to determine the presence of dark spots on the bottom or top of your feet. He carefully considers all potential causes, focusing on vascular disorders, and recommends the best treatment options to address your concerns.


